In a concerning revelation, an expert in the field of obesity has stated that this condition not only affects the body but also has a profound impact on the brain. These changes are said to be irreversible, raising alarming implications for those struggling with or at risk of obesity. In an article by CNN, the expert highlights the gravity of this issue, shedding light on the long-term effects that obesity can have on the brain’s function and structure. With no sign of reversibility, this information serves as a wake-up call to society, urging a greater focus on prevention and intervention strategies to combat the growing obesity epidemic.
Read more about the health news
Introduction
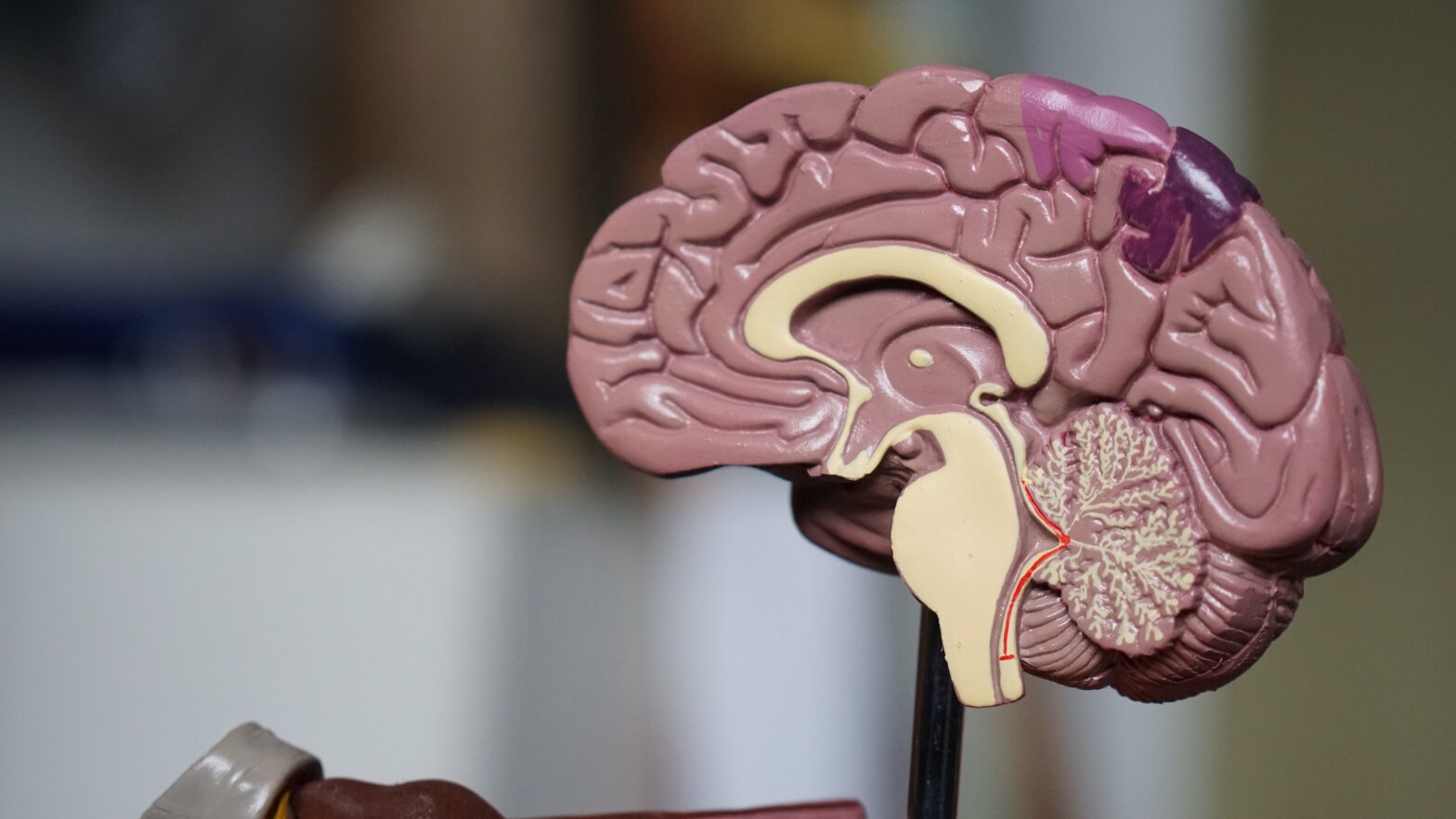
Obesity is a global health concern that affects millions of people worldwide. It is characterized by excessive body fat accumulation, which can lead to various physical health problems such as diabetes, heart disease, and stroke. However, research has also shown that obesity can have a significant impact on the brain, affecting both its structure and function. In this article, we will explore the detrimental consequences of obesity on the brain and discuss potential interventions to mitigate these effects.
The Impact of Obesity on the Brain
Research shows obesity affects brain structure
Numerous studies have demonstrated that obesity can cause alterations in the structure of the brain. One specific finding is that obesity is associated with a reduction in brain volume. Research has shown that individuals with obesity have smaller brain volumes compared to those with healthy weights. These structural changes have been observed in several brain regions, including the prefrontal cortex, hippocampus, and amygdala.
Obesity linked to reduced brain volume
One notable consequence of obesity-related brain changes is the reduced volume of certain brain regions. The prefrontal cortex, which is involved in executive functions such as decision-making and impulse control, tends to be smaller in individuals with obesity. Additionally, the hippocampus, a region critical for memory formation and learning, has been found to have reduced volume in people with obesity. These structural alterations can have a significant impact on cognitive abilities and behavior.
Effects of obesity on brain function
In addition to structural changes, obesity has been found to have detrimental effects on brain function. Research has shown that individuals with obesity often exhibit impaired cognitive function, such as reduced attention, memory problems, and slower information processing. These impairments can significantly impact daily life, making it more difficult for individuals with obesity to perform tasks that require cognitive abilities.
Read more about the health news
Neurological Consequences of Obesity
Increased risk of cognitive decline
Obesity is linked to an increased risk of cognitive decline, a condition characterized by a progressive deterioration of cognitive function. Longitudinal studies have found that individuals with obesity are more likely to experience declines in cognitive abilities, such as memory and executive functions, compared to those with normal weight. The mechanisms underlying this increased risk are not fully understood but may involve the negative impact of obesity on brain structure and function.
Higher likelihood of developing dementia
In addition to cognitive decline, obesity is associated with a higher likelihood of developing dementia, a collective term for various brain disorders that lead to a decline in memory, thinking, and behavior. Multiple studies have found that individuals with obesity have an increased risk of developing dementia, including Alzheimer’s disease, vascular dementia, and mixed dementia. The exact mechanisms linking obesity to dementia are complex and multifactorial, involving both vascular and metabolic pathways.
Obesity and mental health disorders
Obesity is also closely linked to an increased prevalence of mental health disorders. People with obesity are more likely to experience mood disorders, such as depression and anxiety. The relationship between obesity and mental health is bidirectional, with obesity increasing the risk of mental health disorders, and mental health disorders contributing to the development and maintenance of obesity. These comorbidities can further exacerbate the detrimental effects of obesity on brain health.
The Role of Inflammation
Inflammation as a key factor in obesity-related brain changes
In recent years, inflammation has emerged as a crucial factor in obesity-related brain changes. Chronic low-grade inflammation, often present in individuals with obesity, has been shown to contribute to structural and functional alterations in the brain. Inflammatory processes can disrupt cellular communication, induce oxidative stress, and impair neuroplasticity, ultimately leading to cognitive impairments and neurodegenerative diseases.
Chronic low-grade inflammation and its effects on the brain
Chronic low-grade inflammation, characterized by elevated levels of inflammatory markers, such as C-reactive protein (CRP) and interleukin-6 (IL-6), has been found to have detrimental effects on the brain. Studies have shown that elevated levels of inflammatory markers are associated with cognitive decline and an increased risk of dementia. Inflammation in the brain can lead to neuroinflammation, neuronal damage, and the activation of immune responses that further perpetuate inflammation.
Inflammatory markers in obese individuals
Obese individuals often exhibit higher levels of inflammatory markers compared to those with normal weight. Adipose tissue, particularly visceral fat, secretes pro-inflammatory molecules called adipokines, which contribute to systemic inflammation. Additionally, obesity-related metabolic dysregulation, such as insulin resistance and dyslipidemia, can further promote inflammation. These chronic inflammatory processes can have deleterious effects on the brain, contributing to the cognitive impairments observed in individuals with obesity.
Obesity and Brain Development in Children
Early onset obesity and its impact on brain development
Childhood obesity has become a significant public health concern, with long-term consequences for both physical and mental health. Early onset obesity can impact brain development, leading to structural and functional alterations that may persist into adulthood. Studies have shown that children with obesity exhibit reduced cortical thickness and altered white matter integrity, suggesting abnormalities in brain development.
Long-term consequences of childhood obesity on cognitive function
The consequences of childhood obesity on cognitive function can extend into adulthood. Longitudinal studies have found that individuals who were obese during childhood are more likely to experience cognitive impairments later in life, including difficulties with attention, memory, and executive functions. These long-term consequences highlight the importance of early intervention and prevention strategies to mitigate the detrimental effects of childhood obesity on brain health.
Interventions to mitigate obesity-related brain changes in children
Interventions aimed at mitigating obesity-related brain changes in children often involve a multidisciplinary approach. Promoting healthy lifestyles, including regular physical activity and a balanced diet, is essential in preventing and managing childhood obesity. Additionally, early intervention programs that target both physical and mental health can help improve cognitive function and mitigate the long-term consequences of obesity on brain development.
The Gut-Brain Axis and Obesity
Connection between gut health and brain function
The gut-brain axis is a bidirectional communication system between the gut and the brain. Emerging research suggests that the gut microbiota, the collection of microorganisms that reside in the gastrointestinal tract, plays a crucial role in regulating brain function and behavior. Disruptions in the gut microbiota, such as those observed in individuals with obesity, can influence brain health and contribute to cognitive impairments.
Role of gut microbiota in obesity-related brain changes
Obesity has been associated with alterations in the composition and diversity of the gut microbiota. Changes in the gut microbiota can lead to increased gut permeability, allowing the translocation of bacterial products into the bloodstream. These bacterial products, such as lipopolysaccharides (LPS), can trigger immune responses and promote inflammation in the brain. Additionally, the gut microbiota plays a role in the metabolism of nutrients and the production of neurotransmitters that influence brain function.
Potential therapeutic strategies targeting the gut-brain axis
Targeting the gut-brain axis represents a potential therapeutic strategy for mitigating obesity-related brain changes. Probiotics, live bacteria that confer health benefits when consumed, have shown promise in improving cognitive function and reducing inflammation in individuals with obesity. Prebiotics, dietary fibers that promote the growth of beneficial gut bacteria, can also modulate the gut microbiota and potentially improve brain health. Further research is needed to better understand the complex interactions between the gut microbiota and the brain and develop effective interventions.
Obesity, Aging, and Brain Health
Accelerated brain aging in obese individuals
Obesity has been associated with accelerated brain aging, characterized by reductions in brain volume and cognitive decline typically observed in older adults. Neuroimaging studies have revealed that individuals with obesity exhibit brain changes consistent with aging, even in midlife. These age-related alterations can have profound effects on cognitive function and increase the risk of neurodegenerative diseases.
Impact of obesity on neurogenesis and synaptic plasticity
Neurogenesis, the process of generating new neurons, and synaptic plasticity, the ability of synapses to change and adapt, are crucial for brain health and function. Obesity has been found to impair neurogenesis and reduce synaptic plasticity, negatively affecting learning and memory. The underlying mechanisms responsible for these impairments involve chronic inflammation, hormonal dysregulation, and oxidative stress.
Prevention and management strategies for obesity-related brain changes in older adults
Prevention and management of obesity-related brain changes in older adults involve lifestyle modifications and targeted interventions. Regular physical activity, a healthy diet, and weight management are essential for maintaining brain health in older adults with obesity. Additionally, cognitive training programs, social engagement, and the management of comorbidities, such as diabetes and hypertension, can help mitigate the detrimental effects of obesity on brain function and promote healthy aging.
No Sign of Reversibility
Expert opinion on the irreversibility of obesity-related brain changes
According to experts, the brain changes associated with obesity may be irreversible. Although weight loss and lifestyle modifications can improve physical health, the brain may not fully recover from the structural and functional alterations caused by obesity. Research suggests that even after significant weight loss, the brain may continue to exhibit abnormalities, compromising cognitive function and increasing the risk of neurodegenerative diseases.
Challenges in reversing obesity-induced brain damage
The irreversibility of obesity-induced brain damage poses significant challenges for interventions and treatment. The complex and multifactorial nature of obesity-related brain changes, including inflammation, hormonal dysregulation, and metabolic abnormalities, makes it difficult to target specific mechanisms for reversal. Additionally, the long-term effects of obesity on the brain suggest that early intervention and prevention strategies are crucial in mitigating brain damage.
Importance of early intervention and prevention
Given the limited reversibility of obesity-related brain changes, early intervention and prevention strategies are of utmost importance. Public health initiatives should focus on promoting healthy lifestyles and weight management from childhood to minimize the adverse effects of obesity on brain development and function. Education and policy changes that facilitate access to nutritious foods, physical activity, and mental health support can contribute to the prevention and management of obesity.
Addressing the Obesity Epidemic
Public health approaches to tackling obesity
Addressing the obesity epidemic requires a multifaceted and comprehensive approach. Public health strategies aim to create supportive environments that promote healthy lifestyles and facilitate behavior change. These approaches include implementing policies to improve the food environment, such as increasing access to nutritious foods and reducing the marketing of unhealthy products. Additionally, promoting physical activity and creating opportunities for active living are essential in preventing and managing obesity.
Promotion of healthy lifestyles and weight management
Promoting healthy lifestyles and weight management are crucial components of obesity prevention and treatment. Education and awareness campaigns can provide individuals with the knowledge and skills necessary to make informed choices about their diet, physical activity, and overall health. Additionally, behavioral interventions, such as cognitive-behavioral therapy and group support programs, can help individuals adopt sustainable lifestyle changes and maintain a healthy weight.
Role of education and policy changes in preventing obesity
Education and policy changes play a vital role in preventing obesity at both individual and societal levels. Comprehensive health education in schools can equip children with the tools to make healthy choices and develop lifelong habits. Additionally, policy changes that prioritize the availability of nutritious foods in schools, workplaces, and communities can support healthy eating and reduce the prevalence of obesity. Collaborative efforts between healthcare professionals, policymakers, educators, and communities are necessary to address the root causes of obesity and create a healthier society.
Future Directions in Obesity Research
Emerging areas of study in obesity-related brain changes
Obesity research is continually evolving, as scientists strive to understand the complex relationship between obesity and brain health. Emerging areas of study include the role of epigenetics in obesity-related brain changes, the impact of obesity on brain connectivity and network organization, and the identification of novel biomarkers for early detection and intervention. Advancements in imaging techniques and the development of animal models that closely mimic human obesity are expected to further enhance our understanding of the underlying mechanisms.
Innovative interventions for reversing obesity-induced brain damage
Innovative interventions are being explored to mitigate obesity-induced brain damage and promote brain health. These interventions include non-invasive brain stimulation techniques, such as transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS), which have shown promise in improving cognitive function in individuals with obesity. Other novel approaches, such as pharmacological interventions targeting inflammation or gut microbiota, are also under investigation as potential strategies for reversing obesity-related brain changes.
Collaborations and interdisciplinary research in addressing obesity
Addressing the complex issue of obesity requires collaborations and interdisciplinary research. Scientists, clinicians, public health professionals, policymakers, and community stakeholders must work together to develop comprehensive interventions that target the multiple factors contributing to obesity. Collaborative efforts can facilitate the translation of research findings into practical strategies for prevention, intervention, and treatment. By combining expertise from various fields, we can make significant strides in addressing the obesity epidemic and promoting brain health.
In conclusion, obesity has a profound impact on the brain, affecting its structure, function, and development. The detrimental consequences of obesity on the brain range from impairments in cognitive function to an increased risk of neurodegenerative diseases. Inflammation, disruptions in the gut-brain axis, and accelerated brain aging are key factors underlying obesity-related brain changes. Although the reversibility of these changes is limited, early intervention and prevention strategies play a crucial role in mitigating the adverse effects of obesity on the brain. By adopting a comprehensive and collaborative approach, we can address the obesity epidemic and promote brain health for all.